Statin induced Neuropathy |JULY 5, 2020
Befor Diagnosing CIDP STATIN needs to be stoped for a month
Statin Neuropathy Masquerading as Diabetic Tom Brooks Vaughan, MD and David S.H. Bell, MD
Statin-induced neuropathy is increasingly described. Proposedmechanisms include an alteration in cholesterol synthesis, producing a disturbance in the cholesterol-rich neuronal membrane, or in the activity of ubiquinone (coenzyme Q10), a mitochondrial respiratory chain enzyme inhibited by statins leading to neuronal damage (1). The entire class is implicated, and both polyneuropathy and mononeuropathy have been described with improvement or even complete resolution occurring with cessation of therapy (1).In all cases, clinical improvement occurred soon after statinswere discontinued, and in the absence of specific clinical,biochemical, or electrophysiological characteristics, this has become the key diagnostic feature of statin-induced neuropathy.To date, autonomic features accompanying symmetrical neuropathy have not been described.
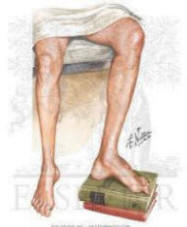
We present an 18-year-old white female with type 1 diabetes for 5 years who, over several months, developed restless legsfollowed by parasthesias, nocturnal diarrhea, fecal incontinence,early satiety, and weight loss. Examination revealed loss ofpinprick sensation to the upper arms and thighs accompaniedby areflexia and loss of vibration sense, a fixed tachycardia,and orthostatic hypotension. Autoimmune demyelinating polyneuropathywas initially suspected due to the relatively rapid onset ofsymptoms and the combination of peripheral and autonomic findings.Neuroelectrophysiological studies showed evidence of axonal,sensory, and motor polyneuropathy but did not meet criteriafor demyelination. Supportive therapy included gabapentin, clonazepam,metoclopramide, metronidazole, cholestyramine, and fludrocortisone.
Before further investigations began, it was noted that the subject had been taking atorvastatin despite very low lipid levels, and it was discontinued.
Within 1 week, her symptoms improved dramatically. Within 6 months, the postural hypotension, diarrhea,and symptoms of gastroparesis had resolved, and all medicines other than insulin were discontinued.
There remained a minimal decrease in vibration sense, areflexia, and loss of sensati onto the wrist and ankle.
Isolated cases of statin-associated neuropathy have been reportedsince 1994
(1). Epidemiological and case-control studies fromthe U.K. and Denmark suggest elevated odds ratios (ORs) of 2.5(95% CI 0.3-14.2) to 3.7 (1.8-7.6), respectively,for the development of neuropathy while on statin therapy .The OR jumped to 26.4 (7.8-45.4) in patients with confirmedneuropathy taking statins for >2 years
The key to diagnosing statin-induced neuropathy is to discontinuethe statin and observe for potential improvement. In conclusion,statins can infrequently cause an idiosyncratic somatic andautonomic neuropathy that, in the diabetic patient, will almostinvariably be attributed to diabetes. Awareness of this associationand a trial removal of the statin could result in restorationof neurological function and a much-improved quality of life in the diabetic patient.top
REFERENCES
1-Backes JM, Howard PA: Association of HMG-CoA reductase inhibitors with neuropathy. Ann Pharmacother 37: 274-278, 2003 Abstract/FREE Full Text
2-Gaist D, Rodriguez LA, Huerta C, Hallas J, Sindrup S: Are users of lipid-lowering drugs at increased risk of peripheral neuropathy? Eur J Clin Pharmacol 56: 931-933, 2001 CrossRefMedline
3-Gaist D, Jeppesen U, Andersen M, Garcia Rodriguez LA, Hallas J, Sindrup SH: Statins and risk of polyneuropathy: a case-control study. Neurology 58: 1333-1337, 2002
65